| |
Hypospadias
- Don't Panic! (and don't circumcise)
Hypospadias is a condition in which the urinary meatus (the pee-hole)
points downward rather than forward. (The word hypospadias comes from
the Greek for "drawn under".)
Photograph of
hypospadias (NSFW)
In the most serious cases the opening may be at the base of the penis
or even behind the scrotum.
Hypospadias occurs in about one boy in 300 in the US.
(but the rate has increased in the last three decades, and is currently
one in 125 - New Scientist, 29 June 2002: exposure during pregnancy to
anti-androgens and oestrogen-mimics generated by industrial pollution
is suspected.) Hypospadias is an absolute contraindication for
circumcision, because the foreskin can be used for its repair, but many
boys with hypospadias are circumcised regardless. It may be iatrogenic, a
consequence of circumcision (picture).
It may be repaired without circumcision, using the Byars' flaps technique
or its "Batman excision"
refinement, or the techniques of the
papers below. Surgical repair is in any case contentious.
|
American Journal of Epidemiology, February 1, 2008.
NEW YORK (Reuters Health) - New research indicates
that genetics rather than the intrauterine environment are mostly
responsible for a relatively common birth defect of the penis. ...
Although hypospadias is one of the most common
birth defects, little is known about its cause, Dr. Tine H. Schnack,
from Statens Serum Institute in Copenhagen, and colleagues note in a
report in the American Journal of Epidemiology.
They investigated genetic and environmental factors
contributing to hypospadias in a study that involved 5,380 boys with
the defect, drawn from a cohort of 1.2 million boys born in Denmark
between 1973 and 2005.
The investigators observed a roughly 51-fold
increased risk of hypospadias in male twin pairs. Moreover, the
presence of a brother, sister or other "first-degree" relative with
hypospadias increased the odds of the defect by nearly 12-fold,
relative to having no close relatives with hypospadias.
The presence of a grandmother or other
"second-degree" relative with hypospadias increased the odds of the
defect by more than 3-fold, while having a more distant third-degree
relative raised the odds of the defect by 33 percent, relative to
having no close relatives with hypospadias.
"These findings indicate that genetic factors have
a principal role in causing familial hypospadias," Schnack and
colleagues conclude.
|
The main problems from hypospadias are
psychological
|
The
Guide to Getting It On
... Hypospadias is usually a minor birth defect
that often looms far more massively in the mind of the guy who's got it
than in mind of a potential partner. There is nothing about hypospadias
that makes a man any less of a man, or any less of a lover, although
sometimes it results in a condition where the penis curves more than
normal.
The real damage from hypospadias is usually the
shame and aloneness that a guy feels when he's growing up. One of the
reasons for feeling so different is because he's often got to sit down
to pee, given how the pee shoots out the side of his penis instead of
the end. The guy knows he's different from other males, and often lives
in terror that others will find out and make fun of him. Of course,
this never happens, given how kind, understanding and uncruel children
are about others who are different...
Aside from feeling like he's got this huge and
horrible secret in his pants, most men with hypospadias have a medical
history where they had to have their penis repeatedly inspected and
examined by this doctor and that. And not being able to leave well
enough alone, surgeons are frequently called in to do what often turns
out to be multiple surgeries. (While medical intervention is sometimes
helpful in certain cases, there are plenty of guys who would have been
far better off if their penis had been spared the surgeon's knife.)
As is the case where any kid grows up feeling his
body is defective, the most important issues to deal with are often the
psychological. Men with hypospadias usually feel great emotional relief
when they can meet and talk to other men who have the same condition.
Fortunately, the Internet is making this much more possible than in
times past.
Men with hypospadias sometimes grow up fascinated
by other guys' penises. This makes perfect sense when you consider how
often their penis gets handled by parents and doctors, often without a
helpful explanation. It also makes sense given how focused a guy with
hypospadias can be about the way his penis is different from other
penises. However, there is no evidence that hypospadias results in a
different sexual orientation unless that's what you were going to do
from the start, hypospadias or not.
As for sex and relationships, the main difference
between a penis with hypospadias and one without is where the cum
shoots out, and that's not going to make a bit of difference to most
women. As one female reader said, "I can name you hundreds of other
things women are more concerned about in a man than if his pee or cum
shoots out straight or from the side--most women wouldn't give a rat's
ass. Only guys worry about things like that."
Rest assured there's no reason why you can't
become a father, so birth control is just as necessary for a man with
hypospadias as for any other guy. The urethral opening for men with
hypospadias is sometimes a little bigger, and some guys are prone to
urinary tract infections, so drinking extra water and peeing after sex
might be a good habit to get into.
Men with hypospadias recommend that you tell a
partner about your hypospadias sometime after you've gotten to know
each other but before you've got your hands in each other's pants. ...
|
Studies describing repair of hypospadias
without circumcision
|
Dewan PA. Distal Hypospadias Repair with Preputial
Reconstruction. J
Paediatr Child Health. 1993; 29:183-184.
Persson-Junemann C, Seemann O, Kohrmann KU,
Potempa D, Junemann KP,
Alken P. Correction of Distal Hypospadias: Ventral Adaptation of the
Prepuce and Meatal Advancement. Urol Int. 1993; 51:216-219.
Hoebeke PB, De Kuyper P, Van Laecke E. 'Batman
Excision' of ventral skin
in hypospadias repair, clue to aesthetic repair (point of technique).
Eur
Urol. 2002; 42(5):520-2.
Gray J, Boston VE. Glanular reconstruction and
preputioplasty repair for
distal hypospadias: a unique day-case method to avoid urethral stenting
and preserve the prepuce. BJU Int. 2003; 91(3):568-70.
Van Dorpe EJ. Correction of distal hypospadias
with reconstruction of the
preputium. Plast Reconstr Surg. 1987; 80(2):290-3.
Terzioglu A, Gokrem S, Aslan G. A modification of
the pyramid procedure:
the correction of subcoronal hypospadias with complete prepuce
(letter).
Plast Reconstr Surg. 2003; 112(3):922-3.
Leclair MD, Camby C, Battisti S, Renaud G,
Plattner V, Heloury Y.
Unstented tubularized incised plate urethroplasty combined with
foreskin
reconstruction for distal hypospadias. Eur Urol. 2004; 46(4):526-30.
|
Is "repair" even necessary?
Intersexed
people take a special interest in hypospadias because if
falls on the Intersex spectrum (at the very beginning, so again, don't
panic). The Swiss Intersex human rights NGO, Zwischengeschlecht.org,
put out a report that includes this:
INTERSEX GENITAL MUTILATIONS
Human Rights Violations Of Children
With Variations Of Sex Anatomy
...
p 15
b) Hypospadias “Repair”
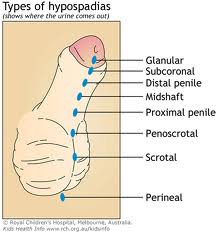
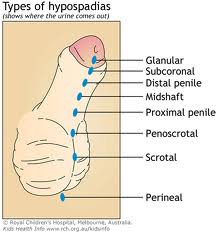
Hypospadias is a medical diagnosis describing a
penis with the urethral opening (“meatus”, or “pee hole”) not situated
at the tip of the penis, but somewhere below on the underside, either
still on the glans (“distal” or “anterior”), or farther below somewhere
on the shaft (“middle”), or on the scrotum (“proximal”, or
“posterior”), due to incomplete tubularisation of the urethral folds
during prenatal formation of the penis (see p. 10 “Genital Development
and Appearance”).
In addition, hypospadias is often associated with
a downward curvature of the penis, especially when erect (“chordee”),
in shape resembling the (mostly internal) structures of the clitoris.
In about 10% of cases, hypospadias is associated with undescended
testes. Sometimes, hypospadias is also associated with an unusually
small penis (“micropenis”). Mostly, hypospadias is associated with a
hooded appearance of the foreskin (untubularised foreskin), again
slightly resembling the clitoral hood.
Hypospadias “repair” surgery aims at “relocating”
the urethral opening to the tip of the penis, and, if applicable, to
straighten the penis. The penis is sliced open, and an artificial
“urethra” is formed out of the foreskin of skin grafts (see Supplement
3 “Medical Textbooks”, p. 77). Switzerland was leading in introducing
hypospadias surgeries in German language European countries after World
War II.228
While in very rare cases hypospadias can be
associated with an urethral opening too small to allow unobstructed
passing of urine, which makes appropriate surgical intervention (and
only such) a medical necessity, and in older boys curvature can
sometimes be associated with pain during (involuntary) erections, which
also constitutes an actual medical problem, these are the only
exceptions to the rule that hypospadias
per se does not constitute a medical necessity for interventions.
Furthermore, since the ongoing 2nd “Hypospadias
Boom” (Supplement 1 “Historical Overview,” p. 59) doctors are so bent
on operating, that in a sample of 500 adult “normal” men presenting for
prostate surgery, 225 men, i.e. 45% were classified as “suffering” from
an “abnormal” position of the meatus – despite no complaints, “normal”
function and lack of awareness of their “abnormality”: “However, all
patients participated in sexual intercourse without problems and were
able to void in a standing position with a single stream,” all were
“without complaints about cosmetic or functional aspects,” even those
with “significant hypospadias.” What’s more, all but one homosexual
patient had fathered children, and even in patients diagnosed with
“significant hypospadias,” 60% of the patients and 55% of their
partners were “unaware of the abnormality.” 229
Hypospadias
“repair” is notorious230
for very high complication rates, e.g. 42%–57%,231 as well as for grave
complications which can result in serious medical
problems where none had been before (for example
urethral strictures have lead to kidney failure requiring dialysis),
and frequent “redo-surgeries”. Tellingly, for more than 30 years,
surgeons have been officially referring to “hopeless” cases of repeat
failed “repair” surgeries as “hypospadias cripples” (i.e. made to a
“cripple” by unnecessary surgeries, not by the condition!).232 However, as a 2012
international medical conference in Switzerland revealed, in medical
publications on hypospadias, “[d]ocumentation on complication rates has
declined in the last 10 years.” 233
...
Footnotes:
228 E.g.
Ernst Bilke, born 1958 in South Germany, was sent to Basel for
paediatric hypospadias “repair”, because the local German doctors
refused to do it, wanting to make him into a girl instead, see Ulla
Fröhling (2003) Leben zwischen den Geschlechtern. Intersexualität –
Erfahrungen in einem Tabubereich, at 90–105
229 J.
Fichtner, D. Filipas, A. M. Mottrie, G. E. Voges, R. Hohenfellner
(1995), Analysis of meatal location in 500 men: Wide variation
questions need for meatal advancement in all pediatric anterior
hypospadias cases, Journal of Urology 154:833-834
230 e.g.
Guido Barbaglia (2010), Failed Hypospadias Repair. How Often Is It, and
How to Prevent It?, http://www.failedhypospadias.com/files/Belgrado2.pdf
231 Pierre
Mouriquand (2006), Surgery of hypospadias in 2006 – Techniques
& outcomes, SymposiumIn ternational de Paris – Surgery of
hypospadias in 2006, slides 13, 15, http://www.
canal-u.tv/video/canal_u_medecine/symposium_international_de_paris_surgery_of_hypospadias_
in_2006_techniques_and_outcomes.2212
232 e.g.
ibid., slide 19
233 Katherine
Pfistermuller, Peter Cuckow (2012), Analysis of Data Quality from 30
Years of Published Data on Hypospadias Outcomes, Programme of the 23rd
Annual Meeting of ESPU, Zurich May 09-12, at 204,
http://www.espu2012.org/images/ESPU_2012_Programme.pdf
|
-
|